Comparative Study of Imrt V/S 3Dcrt
in Postmastectomy Breast Cancer Patients
ABSTRACT
Introduction
This study evaluates the dose distribution of reversed planned tangential beam intensity modulated radiotherapy
(IMRT) compared to standard wedged tangential beam
three-dimensionally planned conformal radiotherapy
(3D-CRT) of the chest wall in unselected post
mastectomy breast cancer patients
Methods
For 20 unselected subsequent post mastectomy breast cancer patients
tangential beam IMRT and tangential beam 3D-CRT plans were generated for
the radiotherapy of the chest wall. The prescribed dose was 50 Gy in 25 fractions. Dose-volume histograms were
evaluated for the PTV and organs at risk. Parameters of the dose distribution were compared using the Student t�
test.
Results
Tangential beam IMRT statistically significantly reduced the ipsilateral mean lung dose by an average of 21% (1129
cGy versus 1437 cGy). In all patients treated on the left side, the heart volume encompassed by the 70% isodose line
(V70%; 35 Gy) was reduced by an average of 43% (5.7% versus 10.6%), and the mean heart dose by an average of 20%
(704 cGy versus 877 cGy). The PTV showed a significantly better conformity index with IMRT; the homogeneity index
was not significantly different.
Conclusions
Tangential beam IMRT significantly reduced the dose-volume of the
ipsilateral lung and heart in
unselected post mastectomy
breast cancer patients.
Introduction
Breast cancer is the most common cancer diagnosed in women worldwide (30). In India the majority
of the patients present in advanced stage of disease at diagnosis, and mastectomy is the
most common treatment followed by adjuvant radiotherapy of the chest wall. In western world as patients presents in
earlier stages so breast conserving surgery followed by
adjuvant radiotherapy
is the treatment of choice.(1)
Most mastectomy series show that more than 50% of
LRF occuron the chest wall, with the mastectomy scar
at greatest risk for recurrence. (59, 34, 58) Therefore, treatment to the chest wall is
recommended for almost all post mastectomy patients.
The second most common site of LRF is the supraclavicular/infra clavicular (axillary apex) region. As many as 33% of
LRF occur in this region, with absolute rates of first failure reported in up to
18% of patients, depending upon extent of axillary involvement
and tumor size.(59,20,50) While supraclavicular/axillary apex failures are uncommon in patients with one to three
positive axillary nodes, failure rates increase in patients with = four positive
nodes. Therefore, post
mastectomy radiotherapy, including a supraclavicular field, is recommended in
patients with = four positive axillary nodes. (53, 26) Post mastectomy radiotherapy
included treatment to the chest wall and
draining lymhatics.
The most commonly used technique to treat the whole breast is currently called a tangent beam. This field
arrangement is designed to minimize radiation exposure of the intra thoracic structures, the heart, and particularly
lung. However, due to the curvature of the breast and chest wall, some volume of lung (and
the
heart in left-sided breast cancers) is included in the radiation beam. In many
studies, inclusion of the internal mammary nodes in a comprehensive chest wall field was standard, although today
routine inclusion of this nodal region is controversial. The anatomical location of the internal mammary nodes,
lying in the intercostal spaces of the first five ribs and crossing the patient�s
midline, increases the volume of the treatment field and the volume of heart at risk for exposure in both
right-and left-sided patients.
Several studies have demonstrated a higher risk of cardiac disease when the internal mammary nodes were
included in the treatment fields. (39, 40, 52, 31)
Several Randomized trials have shown that the radiotherapy of the chest wall is associated with a significantly
increased risk of developing
ipsilateral radiation pneumonitis and lung carcinomas,
radiation carditis, soft tissue and bone sarcomas. (56, 19, 18, 14, 57, 37, 38, 41)Radiation pneumonitis is directly
related to the volume of
lung tissue irradiated. The likelihood of pneumonitis increases when the
tangential fields are combined with the axillary �supraclavicular field and adjuvant chemotherapy. (55) Left sided
post mastectomy patients have significantly increased
risk of cardiac toxicity. Radiation related
pericarditis occurs when the dose to heart is above of 35Gy. (42)
Anthracycline based chemotherapy
also predisposes heart to radiation toxicity. (24).
A variety of dosimetric studies have suggested that
intensity modulated radiotherapy (IMRT)
potentially leads to a more favourable dose distribution compared to three-dimensional
planned conformal radiotherapy (3D-CRT) for the radiotherapy of the whole breast after breast conserving surgery.
(13, 25, 2, 7, 15, 16, 21, 22, 23, 29, 35, 36, 45, 46, 47, 48, 51, 54, 61, 27, 8, 9,
10, 11) Radiotherapy treatment planning for the chest wall are complex due to missing tissue and the presence of
lung tissue within the treatment field. Accurate dose distribution is important
as doses to neighbouring organs at risk, such as
heart, lungs and contralateral breast, needs to be
minimized. (3,4,5) There are many differences between the target volume of the chest
wall and the whole breast. The shape of the target volume of the chest wall is usually shallower compared to the
whole breast. In addition, in stage I-IIa patients the
pectoralis muscle, chest
wall muscles, and ribs may be excluded in the target volume of the whole breast, whereas these
structures are included in the target volume of the chest wall. Due to these differences in the
target volume, results of a dosimetric study of the radiotherapy of the whole breast may not be completely
applicable to the radiotherapy of the chest wall. Dosimetric study of the chest wall
is required to compare IMRT with 3DCRT in post mastectomy patients.
This study evaluates the dose distribution of tangential beam IMRT of the chest wall in post
mastectomy breast
cancer patients compared to tangential beam 3D-CRT.
Material and methods
Patient data
20 consecutive post mastectomy breast cancer patients coming to a tertiary care center were included in the study. A
tangential beam IMRT plan and a standard tangential beam 3D-CRT
plan were generated for the chest wall radiotherapy. Thirteen patients had right-sided breast cancer and seven
left-sided.
The target volumes and the dose prescribed according to the
(International Commission on Radiation Units and
Measurement) ICRU Reports 50 and 62 recommendations. According to
this target volume should be surrounded by the 95% isodose line. The planning target volume for chest wall was
defined according to the
breast cancer atlas for radiation therapy planning
consensus definitions of the Radiation Therapy Oncology Group (RTOG) .The chest wall with the pectoralis muscle,
chest wall muscles, and ribs, were included in
planning target
volume(PTV) and excluded the outermost 3 mm from the superficial skin surface. The heart was defined
as all visible
myocardium, from the apex to the right auricle, atrium, and
infundibulum
of the ventricle. The pulmonary trunk, root of the ascending aorta, and superior vena cava were
excluded.
Treatment techniques
A NCCT-simulation was done in order to optimize target dilineation in the supine position on a carbon breast board
with the ipsilateral arm up and head turned to the contralateral side.
Radio-opaque wires were placed on the mastectomy scar and the clinical boundaries (inferior aspect of clavicular
head, mid sternum, mid axillary line, 2cm below the level of the contralateral
infra-mammary sulcus). A CT scan was performed using 5 mm slice thickness. The CT scanning reference point and
target volumes (PTV) were defined. The 3D-CRT and IMRT plans were
generated using the treatment planning system LinaTech.
A Siemens Oncor linear accelerator with dual photon energy of 6 MV and 15 MV and
multileaf collimator
was used for the treatment. The dose calculation was determined using the �Superposition/ convolution� algorithm. 50
Gy in 25 fractions was prescribed dose.
The beam energy of 6 MV was used for all 3D-CRT and IMRT plans because of the better dose coverage of the chest wall
due the lower penetration power compared to 15 MV.
Tangential beam 3D-CRT
The dose was prescribed to the ICRU reference point which was usually located at the centre of the PTVor at the
intersection of the beam axes. Two tangential parallel opposed beams,
physical wedges (usually 15� or 30�), and a
MLC (multileaf collimator) were used for 3D-CRT. The beam
angles, wedge angles, and beam weighting (usually minimal) were chosen to optimize
coverage of the PTV, while causing less exposure to the ipsilateral lung, heart and
contralateral
breast. Gantry angles ranged from 44 to 56� for the medial fields and from 225� to 235� for
the lateral fields for patients treated on the right side, and from 307� to 325� for the medial fields and from 132�
to 146� for the lateral fields for patients treated on the left side. The fields extended
1.8 cm anteriorly of the chest to provide coverage of the �flash� region.
IMRT technique
The beam orientations and angles of the 3D-CRT plan were used same for the tangential beams of the corresponding
IMRT plan. The PTV for IMRT was the same as used for the 3D-CRT plans
plus an extension into the air anteriorly of the chest of 1.5 cm to ensure appropriate opening of the multileaf
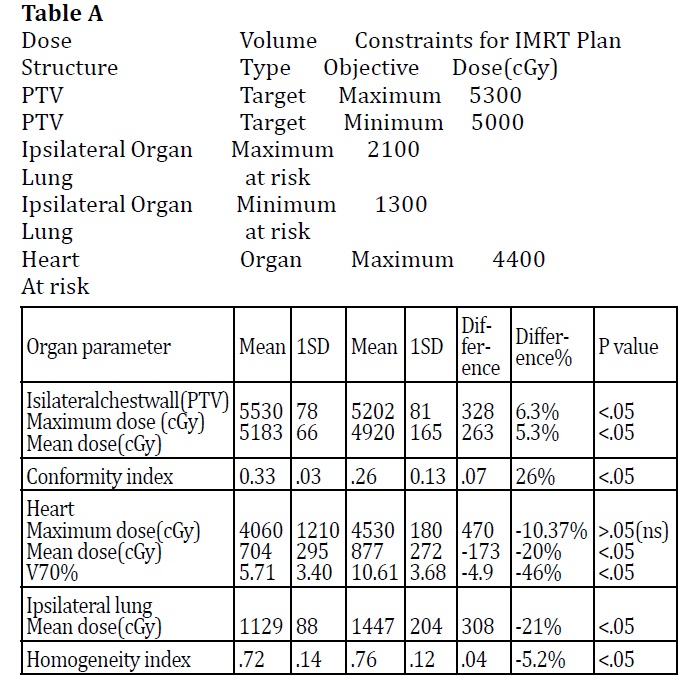
collimator. The dose was prescribed to the PTV, and as initial dose volume constraints
the IMRT prescription table provided by the Linatech treatment planning system (Table A). Tissue inhomogeneities
were considered in the treatment planning optimization process, and the dose calculation was done by using
superposition/ convolution method. A step-and-shoot technique was used.
Dose volume histograms (DVH) of the PTV and organs at risk(OAR) of the 3D-CRT and IMRT plans were
generated and dose parameters compared. The Homogeneity index (HI) was
defined as the fraction of the PTV with a dose between 95% and 105% of the prescribed dose (V95% - V105%). The
Conformity Index (CI) was defined as the fraction of the PTV surrounded by
the reference dose (V95%) multiplied by the fraction of the total body volume covered by the reference PTV dose
((PTV95% /PTV) � (PTV95% /V95%)).
Statistics
IMRT and 3D-CRT plan parameters derived from the same patient were tested for statistically significant difference
using the student� t� P- Value is 0<.05 if Value of t >2.1009 i.e. the difference is significant.
Results
Table B (about here?) compares plan parameters of opposed tangential beam IMRT with conventional 3D-CRT for the
adjuvant radiotherapy of the chest wall in 20 consecutive
breast
cancer patients after mastectomy.
Figure 1(about here?) demonstrates typical dose distributions of an IMRT and 3D-CRT plan of the same patient.
In comparision to 3DCRT the maximum and mean dose for chest wall(PTV) was higher in tangential beam IMRT Plan.
Tangential beam IMRT also improved the conformity index compared to
3D-CRT. The Homogeneity Index was not significantly different between the IMRT and 3D-CRT plans.
Left side treated patients showed a reduction of the V70% (percentage of volume encompassed by the 70% isodose line;
corresponding to the volume receiving =35 Gy) of the heart with an
average of 46% (P < 0.05). The mean heart dose was reduced by an average of 20%. The ipsilateral mean lung dose
was statistically significantly reduced by an average of 21%.
The mean volume and the standard deviation (1SD) of the PTV (chest wall) was 622.0 cm3 (176.7 cm3), of the heart
534.2 cm3 (130.5 cm3), and of the
ipsilateral lung 1150.7 cm3 (254.4 cm3).
Discussion
Several studies have showed a dosimetric benefit of IMRT compared to 3D-CRT for the whole breast in early
breast cancer patients. Comparison of IMRT with 3DCRT in respect to post
mastectomy radiotherapy has not done. In our country patients come in advanced stages when breast conserving surgery
is not possible. So mastectomy is the treatment of choice here. There
are distinct geometric differences between the target volume of the chest wall and the whole breast, and these
differences might have an impact on the resulting dose distribution. This study
was undertaken to evaluate the dose distribution of tangential beam IMRT of the chest wall compared to tangential
beam 3DCRT in unselected
post mastectomy breast cancer patients.
In our study tangential beam IMRT of the chest wall compare to 3D-CRT significantly reduces the ipsilateral lung
dose-volume (D30% by 43%), and heart dose-volume in patients treated on
the left side (V70% by 46%). Clinically it is not possible to estimate the effect of heart dose volume reduction by
the tangential beam IMRT .Radiation associated heart disease involves a
spectrum of clinical diagnosis including pan
carditis pericarditis cardiomyopathy and coronary heart disease
with ischeamic heart disease.
Clinical presentations of radiation induced heart disease have been observed in patients who received therapeutic
doses of about =35 Gy to partial volumes of the heart. Predisposing factors for radiation induced heart disease are
pre-existing cardiovascular disease, smoking, obesity, and hypertension
as well as the use of cardiotoxic agents such as anthracyclines, paclitaxel and trastuzumab. (42, 24) To prevent
radiation toxicity of the heart all measures should be attempted to reduce
cardiac radiation exposure
Increased irradiated volume of the lung causes radiation pneumonitis. Clinically, radiation pneumonitis is
characterized by a chronic cough, fever, and nonspecific infiltrate on chest x-ray. It
usually develops in the first few months after radiotherapy and (for
breast cancer patients) is
usually self-limited, with symptoms lasting an average of 4 weeks. Few patients require any specific treatment.
Changes on x-ray may persist after the resolution of symptoms. (55)
Chemotherapy may cause pulmonary toxicity independently of radiotherapy, and hence combining these
modalities may result in enhanced lung damage. (6) Both the sequencing of chemotherapy
and radiotherapy, radiotherapy treatment technique (which affects the volume of lung treated), and the drugs used
may be important in determining this effect. Thus, careful treatment
planning to limit the volume of treated lung is warranted. When this is done, the risk of pneumonitis is low and
should not restrict the use of PMRT.
An increased risk of secondary tumours has been observed in
breast cancer patients treated with older
radiation techniques, which combined higher radiation dose and larger tissue volumes.The carcinogenic effects of
radiotherapy used for the treatment of breast cancer patients have recently been reviewed.
Second malignancies develop in the radiation field in a small number of cases. The two types of potentially lethal
malignancy that appear in the radiation field most often are
soft tissue and bone sarcomas and lung
cancer. (62)
Sarcomas develop an average of 10 years after irradiation. Therefore, the frequency of
sarcomas
developing in the radiation fields is especially difficult to ascertain for patients treated
with current radiotherapy techniques and equipment. (17) Two Swedish registry studies have suggested that an
increase in the �integral dose� (a combination of radiation dose and treatment
volume) increases the risk of
sarcoma development. (43, 44)
Women with breast cancer are at a 0.3% to 1% per year risk of developing a contralateral breast
cancer. (49, 32) The risk of contralateral breast cancer in several cancer registry case-control
studies was increased slightly in women treated with radiation, probably a result of the small dose of �scatter�
radiation to the opposite breast. (33, 60, 12, 28) This increased risk seems
confined to patients younger than 40 to 45 years old at treatment. In an analysis of data from the Connecticut Tumor
Registry, patients age 45 or younger at exposure had an increased
relative risk of 1.59 (95% confidence interval, 1.07 to 2.36); at an average dose of 1 Gy delivered to the
contralateral breast, the estimated relative risk was 1.21. (61)
Modern radiotherapy techniques as IMRT are likely to reduce the secondary cancer risk by reducing the
lung dose-volume.
Smoking has been shown to significantly increase the risk of second
lung cancer in radiotherapy
patients even if modern radiation techniques were used Prospective studies with long
follow-up times are needed to fully evaluate the cardiac toxicity and secondary
lung cancer risk in breast
cancer patients treated with tangential beam IMRT.
We treat right sided breast cancer patients with 3DCRT and left sided
breast cancer with IMRT as IMRT
is much costlier then 3DCRT and most patients coming to our department cannot afford
IMR.
Conclusions
In post
mastectomy patients tangential beam IMRT significantly reduces the dose-volume of the
ipsilateral lung and dose-volume of the heart in left sided patients compared to tangential
beam 3D-CRT.
Abbreviations
DX%: Dose to X% of the volume (PTV or Organs at risk); IMRT:
Reversed planned intensity modulated radiotherapy; PTV: Planning
target volume; VX%: Percentage of tissue encompassed
by the X% isodose line, representing the volume of tissue that
receives at least 95% of the prescribed dose; 3D-CRT: Threedimensionally
planned conformal radiotherapy.
Legends
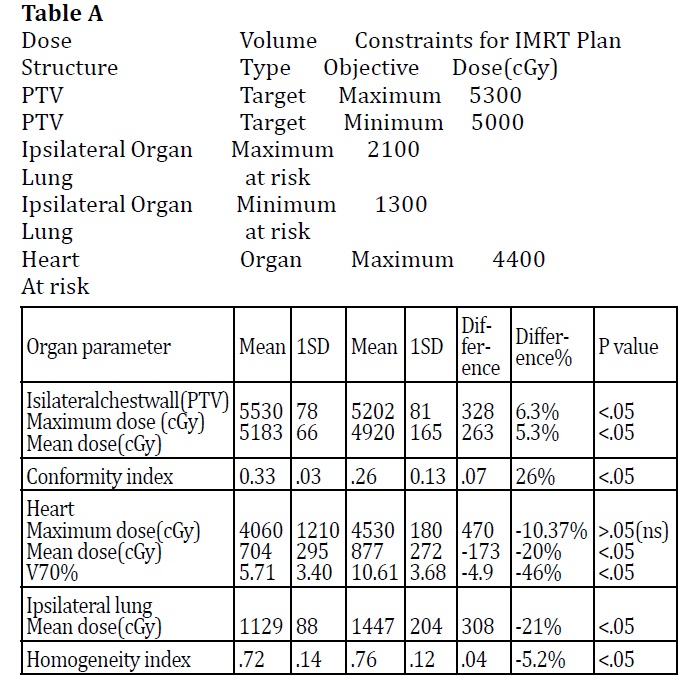
Table B. Relevant plan parameters of tangential beam IMRT versus
tangential beam 3D-CRT of the adjuvant radiotherapy of the chest wall in post mastectomy breast cancer
patients.